Abstract
Exposure to adverse life events is linked to somatic disorders. The study aims to evaluate the association between adverse events at varying life stages and the risk of chronic kidney disease (CKD), a condition affecting about 10% population worldwide. This prospective cohort study included 140,997 participants from the UK Biobank. Using survey items related to childhood maltreatment, adulthood adversity and catastrophic trauma, we performed latent class analysis to summarize five distinct patterns of exposure to adverse life events, namely “low-level exposure”, “childhood exposure”, “adulthood exposure”, “sexual abuse” and “child-to-adulthood exposure”. We used Cox proportional hazard regression to evaluate the association of patterns of exposure to adverse life events with CKD, regression-based mediation analysis to decompose the total effect, and gene-environment-wide interaction study (GEWIS) to identify interactions between genetic loci and adverse life events. During a median follow-up of 5.98 years, 2734 cases of incident CKD were identified. Compared with the “low-level exposure” pattern, “child-to-adulthood exposure” was associated with increased risk of CKD (hazard ratio 1.37, 95% CI 1.14 to 1.65). BMI, smoking and hypertension mediated 11.45%, 9.79%, and 4.50% of this total effect, respectively. Other patterns did not show significant results. GEWIS and subsequent analyses indicated that the magnitude of the association between adverse life events and CKD differed according to genetic polymorphisms, and identified potential underlying pathways (e.g., interleukin 1 receptor activity). These findings underscore the importance of incorporating an individual’s psychological encounters and genetic profiles into the precision prevention of CKD.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is one of the leading contributors to the increasing global burden of disease. It affects around 10% of adults worldwide, causing an annual death toll of 1.57 million in 2022, and is projected to rank among the top five causes of death in 2050 [1, 2]. CKD is linked to a cascade of adverse outcomes, such as electrolyte disturbance, bone mineral disorders, cardiovascular diseases, decreased quality of life, and premature mortality [2, 3]. Consequently, it is imperative to urgently identify the risk factors underlying CKD to enhance its effective prevention and management.
Previous studies indicate that the pathogenesis of CKD is multifactorial, encompassing genetic predispositions, cardiometabolic and inflammatory disorders, as well as lifestyle and behavioral factors, among others [2, 4,5,6]. Psychological distress and psychiatric disorders have also been linked to the onset of CKD. For example, observational and Mendelian randomization research suggests that depression or depressive symptoms are risk factors for CKD [7, 8]. Stress-related disorders contribute to increased susceptibility to CKD progression [9]. While a link has been suggested between adverse life events and cardiovascular as well as autoimmune diseases [10,11,12,13,14], relatively little is known regarding CKD. Regardless, adverse experiences in childhood or adulthood have been reported to influence the occurrence of various illnesses, such as hypertension [15], diabetes [16], and cardiovascular diseases [17, 18], as well as unhealthy lifestyles like smoking and physical inactivity [19], all of which are risk factors for CKD. Studies have also demonstrated that traumatic experiences can adversely affect several physiological pathways, such as altered aging, neuroendocrine system, and immune responses [20, 21], which are known to potentially contribute to the onset of CKD. In real circumstances, people may face psychologically traumatic events throughout life. Exposure to childhood trauma can lead to latent stress vulnerability [22] and act synergistically with adulthood trauma to increase somatic symptoms in later life [23].
In the current study, by leveraging data from the UK Biobank, we investigated the association between patterns of exposure to adverse life events, which were summarized from childhood maltreatment, adulthood adversity, and catastrophic trauma [24, 25], and the subsequent risk of incident CKD. We hypothesized that adverse life events, especially the enduring and recurrent ones, might exert significant influence on the incidence of CKD. In addition, we performed mediation analyses and gene-environment-wide interaction study (GEWIS) to explore the possible explanations for the association between adverse life events and CKD.
Methods
Study population
The prospective cohort study was conducted using data from UK Biobank, a large-scale cohort that recruited around 500,000 participants between 2006 and 2010 [26]. The UK Biobank has collected a comprehensive range of information about participants’ health and well-being, including data on demographic characteristics, socioeconomic status, behavioral and lifestyle factors, environmental exposures, medical conditions, medications, genomic data, and imaging. In particular, information on exposure to adverse life events was obtained from participants who completed an online mental health self-assessment questionnaire in 2016. The UK Biobank offers long-term follow-up on health-related outcomes by linking participant records with death, hospital inpatient, cancer, and primary care records [26].
Among the 502,507 participants in the UK Biobank, we included 146,765 individuals who completed the online mental health survey in 2016. We further excluded 42 participants who withdrew from the study, and 3630 individuals with a baseline estimated glomerular filtration rate (eGFR) less than 60 ml/min/1.73 m2. Considering the potential diagnostic delay of CKD and the risk of reverse causality, we started the follow-up from one year after the online mental health survey and further excluded 1684 participants who were diagnosed with CKD and 412 participants who died prior to or within this year. Thus, 140,997 participants were included for the primary analyses (Supplementary Fig. S1). We derived a genetic analysis cohort (n = 101,879) by further excluding nonwhite participants and those without qualified genomic data.
Assessment of patterns of exposure to adverse life events
The exposure of the current study was pattern of exposure to adverse life events, summarized based on 15 individual items of three domains, namely childhood maltreatment, adulthood adversity, and catastrophic trauma [17, 24, 27]. The three domains included five items each, which were collected in the online mental health survey in 2016. The domain of childhood maltreatment included physical neglect, emotional neglect, sexual abuse, physical abuse, and emotional abuse in childhood [28], using the 5-item Childhood Trauma Screener, designed for adults to rate adverse events that may have happened in childhood [27]. The domain of adulthood adversity included relationship insecurity, physical violence, belittlement, sexual interference, and financial insecurity after 16 years of age [17], using a questionnaire with the same structure of the Childhood Trauma Screener [27]. Catastrophic trauma was defined as harmful events that had the potential to cause post-traumatic stress disorder [29], including being victim of sexual assault, being victim of physically violent crime, experiencing serious accident, witnessing sudden violent death, and being involved in combat or war [27]. We did not include being diagnosed with a life-threatening illness as an item for catastrophic trauma, considering its high correlation with Charlson’s comorbidity index, which is a significant risk factor for CKD.
For items included in the domains of childhood maltreatment and adulthood adversity, each item has the potential responses of 0, 1, 2, 3, and 4 corresponding to “never true”, “rarely true”, “sometimes true”, “often true”, and “very often true”. For catastrophic trauma, responses were coded as 0, 1, and 2 corresponding to “never”, “Yes, but not in the last 12 months”, and “Yes, within the last 12 months”. Each item was coded as 1 for exposure to the event or 0 for no exposure to the event according to predefined thresholds (Supplementary Table S1). For the evaluation of specific domains, we dichotomized childhood maltreatment, adulthood adversity, and catastrophic trauma as “yes” if at least one item of a specific domain was positive or “no” if none of the items was positive in this domain.
Considering the correlation between the individual items of the domains, and the fact that there can be different combinations of adverse life events at varying periods of life course, we used latent class analysis (LCA) to derive patterns of exposure to adverse life events based on all 15 individual items. With the underlying assumption that membership in unobserved groups can be explained by assessment indicators, LCA is a statistical procedure used to identify different subgroups that share certain outward characteristics [30]. To determine the number of classes, we fitted the different LCA models with two to eight latent classes and calculated several statistical metrics: Bayesian information criteria (BIC) and sample-size adjusted BIC, which balance model fit and simplicity, with lower values indicating better fit; Entropy, which measures the separation between classes, with a value close to 1 being ideal but potentially leading to over-fitting; and average latent class probabilities, with 0.8 being acceptable [30,31,32] (Supplementary Fig. S2). In our analysis, BIC and sample-size adjusted BIC decreased as the number of classes increased from two to eight, but the change was less pronounced with more than five classes. Although the Lo–Mendell–Rubin adjusted likelihood ratio test (LRT) remained statistically significant (P < 0.05), including too many classes could lead to the risk of overfitting and compromise the interpretability of the model [33]. Therefore, taking into account both statistical metrics and clinical interpretability [32], we selected the five-class strategy. According to the item-response probabilities that were at least twice the average probabilities in all participants, class 1 was characterized as “low-level exposure”, class 2 as “childhood exposure”, class 3 as “adulthood exposure”, class 4 as “sexual abuse”, and class 5 as “child-to-adulthood exposure” (Fig. 1).
A Average percentage of participants with exposure to individual items of adverse life events in the whole cohort and the corresponding percentages in different patterns. B Ratios of percentage of participants with exposure to individual items of adverse life events in different patterns to the average percentage in the whole cohort.
Ascertainment of CKD
CKD cases were identified by codes of the International Classification of Disease version 9 (ICD-9) and ICD-10 through linkage to hospital inpatient records or national death registries [34], or algorithmically defined outcome for end-stage renal disease (ESRD) based on hospital admission records, self-report verified by nurse interview, or death certificate records in the UK Biobank (Diagnostic codes shown in Supplementary Table S3) [35]. The end of follow-up was the date of first CKD diagnosis, the date of death, or 30 November 2022, whichever came first.
Covariates
Covariates included sex, ethnicity, education levels, household income, employment status, Townsend Deprivation Index, smoking status, diet, alcohol consumption, physical activity and body-mass index (BMI), which were collected at baseline, and information on age, hypertension, diabetes, depression, anxiety, substance misuse and Charlson index collected until November 2016. Data fields used in this study and detailed definitions are listed in Supplementary Tables 3 and 4. We divided ethnicity into White, Black, Asian, mixed and others as reported by the participants; household income into ultra-high (>₤100,000), high (₤52,000 to 100,000), medium (₤18,000 to 51,999), and low (< ₤18,000) levels [36, 37]; employment status into employed (in paid employment or self-employed, retired, doing unpaid or voluntary work, or being full or part-time students) and unemployed; and educational level into one category of college or university degree, one category of A levels/AS level, O levels/GCSEs or CSEs, and one category of NVQ or HND or HNC or other professional qualifications. Townsend Deprivation Index was quantified according to the postal code of participants based on employment, car ownership, home ownership, and household overcrowding [38, 39]. Smoking status was classified as current, previous or never. Diet was defined as ideal based on favorable intake of at least five of the following dietary components: fruit, vegetable, whole grains, fish, diary, vegetable oils, refined grains, processed meat, unprocessed meat and sugar-sweetened beverages [40]. Physical activity was defined as ideal if participants had at least 150 min/week moderate, 75 min/week vigorous, or 150 min/week mixed (moderate and vigorous) activities, as poor if participants did not perform any moderate or vigorous activity, and as intermediate otherwise [40]. BMI was categorized into obesity (BMI ≥ 30 kg/m2), overweight (BMI between 25 and <30 kg/m2), normal weight (BMI between 18.5 and <25 kg/m2), and underweight (BMI < 18.5 kg/m2). Diagnoses of hypertension, diabetes, depression, anxiety, and substance misuse were obtained through linkage to hospital inpatient records. In addition, hypertension and diabetes were further identified by participants’ self-reported medical conditions and medications (Supplementary Table S3). Comorbidities of Charlson Comorbidity Index were identified according to coding algorithms for ICD-10 diagnoses [41] and Charlson Comorbidity Index was classified into three categories: ≥3, 1 to 2, and 0 [42]. Missing values were imputed by the mean for continuous variables and were coded as an “unknown” category for categorical variables.
In the genetic analysis cohort, we calculated polygenic risk score (PRS) for estimated glomerular filtration rate (eGFR) using GWAS by Wuttke and colleagues as the base data [43]. Genotyping in the UK Biobank was performed using the UK BiLEVE AxiomTM Array and UK Biobank Axiom array from Affymetrix. The analysis of genetic susceptibility was restricted to participants of White British ancestry who had passed data quality control. In order to select valid instrumental variables (IVs), palindromic SNPs (i.e., SNPs with A/T or C/G at intermediate frequencies) were removed [44]. Finally, about 3.2 million pruned SNPs (r2 < 0.1, in the 250 kb region, with p value less than 0.01) were retained for PRS calculation by summing up the reference alleles for each SNP weighted by the summary regression coefficient for eGFR [45]. The PRS was calculated using PLINK1.9 software [44].
Statistical analyses
Primary analyses
Continuous variables were presented as mean with standard deviation and compared by analysis of variance if normally distributed, and as median with interquartile range (IQR) and compared using Kruskal–Wallis tests if not normally distributed. Categorical variables were reported as percentage and compared by Chi-square test. We conducted Cox proportional hazard regression model to obtain the hazard ratio (HR) of incident CKD in relation to adverse life events. Prespecified confounders were adjusted for in the analysis, including age, ethnicity (White, Black, Asian, mixed or other), educational level, employment status (employed, unemployed, or unknown), Townsend deprivation index, BMI categories (underweight, normal weight, overweight, obesity, or unknown), alcohol consumption (ideal, poor or unknown), diet habit (ideal, poor or unknown), physical activity (ideal, intermediate, poor or unknown), history of hypertension (yes or no), history of diabetes (yes or no), history of depression (yes or no), history of anxiety (yes or no), history of substance misuse (yes or no), and Charlson Comorbidity Index categories (≥3, 1 to 2 or 0). In the genetic analysis cohort, we additionally adjusted for polygenic risk categories for CKD (high, medium and low risk stratified by tertiles of PRS).
Subgroup and sensitivity analyses
We performed subgroup analyses by sex, age (<65 years and ≥65 years), history of hypertension, history of diabetes, and polygenic risk categories for CKD. We also introduced interaction terms between these variables and exposure to adverse life events to the original models to evaluate the statistical significance of potential effect modification. Models with and without the interaction terms were compared using likelihood ratio test.
To evaluate the robustness of the findings in the current study, the following sensitivity analyses were conducted: (1) removing CKD cases diagnosed within the first two years of the online mental health survey; (2) conducting Cox proportional hazard regression model using age at follow-up as time scale; (3) using Fine and Gray competing risk model to estimate subdistribution HRs with death as the competing risk; (4) conducting Cox model after multiple imputation for missing covariates where chained equations multiple imputations were conducted using chained equations with five imputations; (5) conducting Cox model adjusting for more detailed categorization of confounders, including household income (>₤100,000, ₤52,000 to 100,000, ₤31,000 to 51,999, ₤18,000 to 30,999, and <₤18,000), smoking status (current smoker, previous smoker with ≥20 pack-years, previous smokers with <20 pack-years who quitted smoking within 15 years, other previous smokers, and never smokers) [46], and Charlson Comorbidity Index (≥5, 4, 3, 2, 1, or 0); (6) deriving pattern of exposure to adverse life events according to different combinations of the individual items included in the three domains: with adverse life event events in both childhood and adulthood, with adverse life events only in childhood, with adverse life events only in adulthood, and with no adverse life events; and (7) assessing the negative impact of different patterns of exposure to adverse life events on the risk of CKD using accelerated failure time (AFT) model, in which Weibull, log-logistic and Gompertz distributions were tested, and log-logistic model was selected based on lowest AIC value.
Mediation analyses
We conducted regression-based mediation analyses to decompose the total effect of adverse life events on CKD that is mediated by known CKD risk factors using CMAverse R package, which supports the evaluation of the mediation effects of continuous, binary, and nominal variables on survival outcomes [47]. The outcome was regressed on patterns of exposure to adverse life events, mediators and confounders using Cox proportional hazard regression model, whereas the mediators were regressed on patterns of exposure to adverse life events and confounders using logistic or multinomial regression as appropriate. No interaction was considered between the exposure and mediators. The point estimate of each effect was obtained by imputing counterfactuals directly [47]. 95% CIs were obtained by bootstrap estimation with 10,000 boots.
GEWIS and functional annotation
The effects of gene-by-pattern of exposure to adverse life events interaction on CKD risk were estimated by Cox proportional hazard regression model, adjusting for age, sex, and the first 10 principal components [48]. The genetic additive (ADD) models were used, the genotype was recoded as 0, 1, and 2 according to the number of risk alleles. High-quality SNPs were selected with call rates >0.90, Hardy–Weinberg equilibrium exact test P-values > 0.001, and minor allele frequencies >0.01 [49]. The threshold for significant and suggestive interactions were P < 5 × 10–8 and P < 1 × 10–5, respectively [50]. Circular Manhattan plots and quantile-quantile (QQ) plots were used to present the deviation of the observed P values from the null hypothesis. The modifiable effect of each suggestive SNP was further confirmed by Cox proportional hazard regression models stratified by the status of carrying risk alleles or not.
After identifying the potential interactive SNPs, we conducted following bioinformatics analyses to explore the function of these variants. First, gene annotation was performed by FUMA (v1.6.0) [51]. Lead SNPs and SNPs in linkage disequilibrium (LD) with the lead SNPs were mapped to genes based on positional information (within 10 kb region). Europeans from 1000 genomes project were used as reference panel in calculating LD score. Herein, lead SNPs were defined as SNPs independent from other lead SNPs (LD of r2 < 0.1, P < 1 × 10–5), SNPs in LD were defined as SNPs within a 250 kb window and r2 ≥ 0.6. Enrichment analysis for Gene Ontology (GO) annotation was performed with MsigDB C5 gene sets as reference using the methodology described before [52]. Second, we searched for Human Kidney eQTL Atlas database and evaluated the potential effects of suggestive SNPs on the transcriptomic regulation of surrounding genes (cis-eQTL) or distal genes (trans-eQTL) in the human kidney [53]. Third, we searched for phenotypic-level associations with the suggestive SNPs in GWAS Catalog database [54].
R software (version 4.1.2), PLINK (version 1.9) and Mplus (version 7.4) were used in the statistical analyses. A two-sided p < 0.05 was considered statistically significant.
Ethical approval
The study was conducted using the UK Biobank data, with application number 54803. The UK Biobank has obtained ethical approval from the NHS National Research Ethics Service (16/NW/0274). All the UK Biobank participants gave written informed consent. This study was approved by the biomedical research ethics committee of West China Hospital (2019-1171).
Results
Participants’ characteristics
Among the 140,997 participants, median age was 64.79 years (IQR 57.96 to 69.96), 44% were males, and 82% participants had experienced at least one type of the studied adverse life events. As listed in Table 1, compared with “low-level exposure”, participants experiencing more adverse life events were younger; more likely to be nonwhite, in low-income category, unemployed, obese, and current smokers; and more likely to have an unhealthy alcohol consumption habit and a history of hypertension, diabetes or depression.
Association between adverse life events and CKD incidence
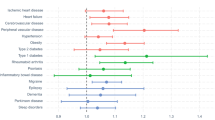
Over a total of 843,232.5 person-years of follow-up (median 5.98 years) after the 2016 online mental health survey, 2734 CKD cases were identified, corresponding to an incidence of 1.94% and an incidence rate of 3.24 per 1000 person-years. We first conducted Cox proportional hazard regression model to evaluate the association between the three individual domains of adverse life events with the risk of CKD. We found that the presence of childhood maltreatment was significantly associated with the risk of incident CKD (HR 1.10, 95% CI 1.002 to 1.21, P < 0.001), while the associations between the presence of adulthood adversity (HR 1.17, 95% CI 0.99 to 1.17, P = 0.051) or catastrophic trauma (HR 1.05, 95% CI 0.97 to 1.13, P = 0.241) and incident CKD were not statistically significant. We then explored the impact of patterns of exposure to adverse life events on the risk of CKD. As shown in Fig. 2, compared with “low-level exposure”, the “child-to-adulthood exposure” was associated with 37% increased risk of CKD after adjusting for potential confounders (HR 1.37, 95% CI 1.14 to 1.65; P < 0.001). Other patterns of exposure to adverse life events did not show significant associations with the risk of incident CKD (Fig. 2).
The hazard ratios obtained from Cox proportional hazard regression models are shown. Model 1 was adjusted for age, sex and ethnicity. Model 2 was adjusted for confounders in Model 1 and education level, income level, employment status, Townsend deprivation index, BMI categories, smoking status, alcohol consumption, diet habit, and physical activity. Model 3 was adjusted for confounders in Model 2 and history of hypertension, diabetes, depression, anxiety, substance misuse, and Charlson comorbidity index categories. Model 4 was adjusted for confounders in Model 3 (without ethnicity) and polygenic risk score for estimated glomerular filtration rate. * Analyses were conducted in the genetic analysis cohort with qualified GWAS data. HR hazard ratio, CI confidence interval.
In subgroup analyses (Fig. 3), the association for the “child-to-adulthood exposure” pattern was only significant in women, in those under 65 years of age, and in participants with lower polygenetic risk for decreased kidney function. However, interactions were only statistically significant between age group and polygenetic risk category with patterns of exposure to adverse life events. Besides, we noticed that the “childhood exposure” pattern was associated with the risk of CKD in participants at younger age and those with lower polygenetic risk for CKD.
The hazard ratios obtained from Cox proportional hazard regression models are shown. Models were adjusted for confounders, including age, sex, ethnicity, education level, income level, employment status, Townsend deprivation index, BMI categories, smoking status, alcohol consumption, diet habit, physical activity, history of hypertension, diabetes, depression, anxiety, substance misuse, and Charlson comorbidity index categories.
In sensitivity analyses (Supplementary Table S5), the results were similar, namely that the association between “child-to-adulthood exposure” pattern and CKD remained significant after excluding CKD cases diagnosed within the first two years of online mental health survey (HR 1.41, 95% CI, 1.17 to 1.69, P < 0.001), in Cox proportional hazard regression model using age as time scale (HR 1.35, 95% CI 1.12 to 1.62, P = 0.001), in Fine-Gray model considering death as a competing risk (HR 1.34, 95% CI 1.12 to 1.62, P = 0.002), after conducting multiple imputations for missing covariates (HR 1.33, 95% CI 1.11 to 1.60, P = 0.002), and after adjusting for more detailed categorization of confounders (HR 1.34, 95% CI 1.11 to 1.61, P = 0.002). Based on the presence of childhood and/or adulthood adverse life events, we also categorized the participants as with no exposure to adverse levents, exposure to adverse life events in childhood only, exposure to adverse life events in adulthood only, and lifetime exposure. Compared with those with no exposure to adverse life events, lifetime exposure was still associated with increased risk of CKD, although the point estimate of HR diminished slightly (HR 1.18, 95% CI 1.06 to 1.32, P = 0.004). Finally, AFT analysis showed that the adjusted time ratio after adjustment for confounders was 0.84 (95% CI, 0.75 to 0.93; P = 0.001) for the “child-to-adulthood exposure” pattern, as compared to low level of exposure, indicating that a prolonged exposure to adverse life events significantly accelerated the onset of CKD by a factor of 0.84.
Mediation analyses
Mediation analyses showed that several known risk factors for CKD mediated some proportion of the association between the “child-to-adulthood exposure” pattern and CKD (Table 2). BMI turned out to be the most prominent mediating factor, which mediated 11.45% (95% CI 6.39% to 28.58%) of the total effect. Besides, we also observed significant mediating effects for smoking (9.79%) and hypertension (4.50%). However, diet and diabetes had no significant mediating effect.
GEWIS and functional annotation
GEWIS identified 154 suggestive SNPs interacting with the “child-to-adulthood exposure” pattern on the risk of CKD incidence (Supplementary Table S6). Two types of P value plots, namely Circular Manhattan plots and QQ plots, are shown in Supplementary Fig. S4. When stratified by genotypes, compared to “low-level exposure”, the estimated effect size of the “child-to-adulthood exposure” pattern on risk of CKD was generally higher among individuals carrying a risk-allele (heterozygotes or homozygotes) than in homozygous non-risk allele carriers, despite of wider 95% CI (Fig. 4 and Supplementary Table S7).
These suggestive SNPs mapped to 53 genomic risk loci (Supplementary Table S8) and 1602 genes (Supplementary Table S9). These mapped genes were enriched for interleukin 1 receptor activity (adjusted P = 0.0001) and cytokine receptor activity (adjusted P = 0.02) (Supplementary Table S10). The genomic risk loci containing rs11676124 was a kidney eQTL for SLC9A4 gene (odds ratio 1.22, 95% CI 1.14 to 1.31, P = 2.46 × 10–8), which was reported to be associated with interleukin 1 receptor-like 1 (IL1R1) levels in CKD (Supplementary Table S11) [55].
Discussion
In this cohort study, based on data from the UK biobank, we investigated the association between patterns of exposure to adverse events in childhood and adulthood and the risk of new-onset CKD. To our knowledge, we are among the first to explore the link between exposure patterns to 15 individual items of adverse life events spanning from childhood to adulthood and the risk of CKD. Generally, our findings mount to the accumulating evidence demonstrating that adverse and traumatic experiences with potential mental impact may elevate the risk of somatic disorders, and extend previous findings in several ways.
Firstly, we provided evidence showing that prolonged exposure to adverse life events from childhood to adulthood is associated with an increased risk of CKD and explored potential explanations for such an association. Adverse experiences have been reported to be associated with several diseases, such as psychiatric disorders [56], hypertension [15], diabetes [16], cardiovascular diseases [17], and cancer [57], as well as pathogenic pathways, including accelerated aging [29], dysregulation of neuroendocrine stress response axes (e.g., the hypothalamic-pituitary-adrenal axis) [21], and compromised immunity and inflammation process [58, 59]. Herein, we found that a proportion of the association between “childhood-to-adulthood exposure” to adverse life events and CKD can be attributed to the mediation of BMI, smoking, and hypertension. Besides, through GEWIS, a useful approach to explore biological pathways [50, 60] and identify novel loci associated with the disorders [61,62,63], we identified 154 suggestive SNPs which are enriched in pathways involving inflammatory process, e.g., interleukin 1 receptor and cytokine receptor activity. Notably, we identified a kidney eQTL for the gene SLC9A4, which was reported to be associated with interleukin 1 receptor-like 1 levels in CKD [55]. Previous studies have reported the pro-inflammatory effects of cytokines, like IL-6, IL-1 and CXCR4, in the pathophysiology of CKD, including worsening of renal insufficiency and accumulation of neutrophils and macrophages, followed by inflammatory injury in cardiorenal diseases and stimulation of kidney fibrosis [64,65,66]. Further studies are needed to confirm the role of the above-mentioned potential mechanisms.
Secondly, different magnitude was noted in the associations between different patterns of exposure to adverse life events and CKD, which underlines the necessity to consider the interplay of different adverse events at varying life stages. A specific pattern “child-to-adulthood exposure”, identified by LCA across a wide spectrum of adverse life events, was associated with an increased risk for developing CKD. The use of LCA was triggered by the finding that adverse life events can occur concomitantly and that adverse life events at an earlier age may change the likelihood of experiencing other adverse events later, making it difficult to clarify the independent effect of a single type of event. LCA allows the identification of unobserved or “latent” groups inferred from the patterns of the observed indicators, on the assumption that the observed distribution of the indicators is the result of a finite latent mixture of underlying distributions [32]. It is noteworthy that, using data from the Washington State 2011 Behavioral Risk Factor Surveillance System, Hajat and colleagues [25] summarized latent classes of “Consistently High”, “Adult Interpersonal Victimization”, “High to Low”, “Repeat Sexual Victimization” and “Consistently Low”, similar to the current study, with an additional class “Substance Abuse and Incarceration”. This confirms the feasibility of jointly evaluating co-occurring adverse life events.
Thirdly, our study identified specific subgroups of individuals who may be particularly susceptible to the potential impact of adverse life events on the development of CKD. We observed significant associations between child-to-adulthood exposure to adverse life events and CKD in women, individuals under the age of 65, individuals without diabetes, and individuals with lower genetic risk for developing CKD. This can be attributed to different reasons. First, differences exist in the adaptation of exposure to adverse life events among subgroups of population. Women with higher adverse childhood experiences have been shown to display less habituation of cardiovascular responses after stress task than men [67]. Aging, along with alteration in sex-related hormones, may also play a role [68]. Second, the subjective perception of the adverse life events and the threshold of stress response to trigger consequent health consequence varies. Men and women tend to report different types and numbers of adverse life events [69]. Besides, post-traumatic stress disorder occurs at a higher rate in women than in men following childhood abuse [70]. Third, it is possible that adverse life events might not be as strong risk factors for CKD as other known risk factors. As a result, significant association was only noted among individuals without diabetes and those with lower genetic risk for CKD. This is consistent with our previous reports showing that strong risk factors for CKD, like high level of testosterone, advanced age, and comorbidity of diabetes, might overshadow the impact of moderate behavioral factors (e.g., habitual consumption of coffee and unhealthy sleep) [50, 71]. Regardless, the findings revealed by subgroup analyses can facilitate more effective screening and preventive strategy in targeted populations at high risk for early diagnosis and management of CKD. In addition, we found that if exposed to adverse life events in childhood or adulthood alone, the risk for CKD was not significantly different from the “low-level exposure” pattern. This implies that, while preventing adverse life events over the life course is of great importance, avoidance of persistent or recurrent exposure to adverse life events is potentially useful for the prevention of future CKD, even for individuals who might have experienced such events before.
The strengths of our study include usage of data from a large, community-based cohort, identification of patterns of exposure to adverse life events from childhood to adulthood, and identification of possible mechanisms for the link between adverse life events and CKD, adding knowledge to CKD prevention in an era of big data. Meanwhile, the study has some limitations. Firstly, retrospective collection of information of adverse life events using an online questionnaire may introduce recall bias. Previous studies have reported moderate agreement between retrospective and prospective assessment of adverse childhood experiences, showing that retrospective assessment of adverse life events cannot be assumed to invalidate results [72, 73]. However, considering that information on adverse life events in childhood was collected many years after the actual exposure in the UK Biobank, validation of the present findings using prospectively collected data on adverse life events throughout childhood to adulthood is warranted. Secondly, when deriving patterns of exposure to adverse life events, we did not incorporate the severity of the individual life events. This can lead to partial loss of information. Thirdly, the relatively small sample size in subgroup analyses could have limited statistical power to detect significant differences. The small sample size of non-white participants might also have hampered the generalizability of the main findings to ethnic groups other than white.
To conclude, prolonged exposure to adverse life events is associated with increased risk of CKD. This study also underscores the necessity of considering the interplay of different adverse experiences at varying life stages when assessing the impact of adversities on health outcomes. The study has implications for the precision prevention of CKD based on personal experience of adverse life events and genetic profiles. Besides, the potential pathways revealed by GEWIS warrants further exploration of the mechanism of adversity-CKD association.
Data availability
The data supporting the findings of this study can be applied from the UK Biobank (https://www.ukbiobank.ac.uk/).
Code availability
The R code used in the study is available from the corresponding author upon request.
References
GBD 2021 Forecasting Collaborators. Burden of disease scenarios for 204 countries and territories, 2022-2050: a forecasting analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2204–56.
Kalantar-Zadeh K, Jafar TH, Nitsch D, Neuen BL, Perkovic V. Chronic kidney disease. Lancet. 2021;398:786–802.
Chen J, Li C, Bu C, Wang Y, Qi M, Fu P, et al. Global burden of non-communicable diseases attributable to kidney dysfunction with projection into 2040. Chin Med J. 2024. https://doi.org/10.1097/CM9.0000000000003143
Yin T, Chen Y, Tang L, Yuan H, Zeng X, Fu P. Relationship between modifiable lifestyle factors and chronic kidney disease: a bibliometric analysis of top-cited publications from 2011 to 2020. BMC Nephrol. 2022;23:120. https://doi.org/10.1186/s12882-022-02745-3
Kelly JT, Su G, Zhang L, Qin X, Marshall S, González-Ortiz A, et al. Modifiable lifestyle factors for primary prevention of CKD: a systematic review and meta-analysis. J Am Soc Nephrol. 2021;32:239–53.
Khan A, Turchin MC, Patki A, Srinivasasainagendra V, Shang N, Nadukuru R, et al. Genome-wide polygenic score to predict chronic kidney disease across ancestries. Nat Med. 2022;28:1412–20.
Park S, Lee S, Kim Y, Lee Y, Kang MW, Kim K, et al. Causal effects of positive affect, life satisfaction, depressive symptoms, and neuroticism on kidney function: a Mendelian randomization study. J Am Soc Nephrol. 2021;32:1484–96.
Liu M, Zhang Y, Yang S, Wu Q, Ye Z, Zhou C, et al. Bidirectional relations between depression symptoms and chronic kidney disease. J Affect Disord. 2022;311:224–30.
Su G, Song H, Lanka V, Liu X, Fang F, Valdimarsdóttir UA, et al. Stress related disorders and the risk of kidney disease. Kidney Int Rep. 2021;6:706–15.
Suglia SF, Koenen KC, Boynton-Jarrett R, Chan PS, Clark CJ, Danese A, et al. Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation. 2018;137:e15–e28.
Vaccarino V, Goldberg J, Rooks C, Shah AJ, Veledar E, Faber TL, et al. Post-traumatic stress disorder and incidence of coronary heart disease: a twin study. J Am Coll Cardiol. 2013;62:970–8.
Bookwalter DB, Roenfeldt KA, LeardMann CA, Kong SY, Riddle MS, Rull RP. Posttraumatic stress disorder and risk of selected autoimmune diseases among US military personnel. BMC Psychiatry. 2020;20:23. https://doi.org/10.1186/s12888-020-2432-9
Bengtsson J, Rieckmann A, Carstensen B, Svensson J, Jørgensen ME, Rod NH. Trajectories of childhood adversity and type 1 diabetes: a nationwide study of one million children. Diabetes Care. 2021;44:740–7.
Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009;71:243–50.
Obi IE, McPherson KC, Pollock JS. Childhood adversity and mechanistic links to hypertension risk in adulthood. Br J Pharmacol. 2019;176:1932–50.
Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, et al. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prev Med. 2015;48:345–9.
Cao X, Zhang J, Ma C, Li X, Kuo CL, Levine ME, et al. Life course traumas and cardiovascular disease-the mediating role of accelerated aging. Ann N Y Acad Sci. 2022;1515:208–18.
Wang W, Liu Y, Yang Y, Jiang W, Ni Y, Han X, et al. Adverse childhood and adulthood experiences and risk of new-onset cardiovascular disease with consideration of social support: a prospective cohort study. BMC Med. 2023;21:297. https://doi.org/10.1186/s12916-023-03015-1
Bourassa KJ, Moffitt TE, Harrington H, Houts R, Poulton R, Ramrakha S, et al. Childhood adversity and midlife health: shining a light on the black box of psychosocial mechanisms. Prev Sci. 2023;24:817–28.
Agorastos A, Pervanidou P, Chrousos GP, Bake DG. Developmental trajectories of early life stress and trauma: a narrative review on neurobiological aspects beyond stress system dysregulation. Front Psychiatry. 2019;10:118. https://doi.org/10.3389/fpsyt.2019.00118
Ehlert U. Enduring psychobiological effects of childhood adversity. Psychoneuroendocrinology. 2013;38:1850–7.
Simon L, Admon R. From childhood adversity to latent stress vulnerability in adulthood: the mediating roles of sleep disturbances and HPA axis dysfunction. Neuropsychopharmacology. 2023;48:1425–35.
Barends H, van der Wouden JC, Claassen-van DesselN, Twisk J, van der Horst HE, Dekker J. Potentially traumatic events, social support and burden of persistent somatic symptoms: a longitudinal study. J Psychosom Res. 2022;159:110945. https://doi.org/10.1016/j.jpsychores.2022.110945
Chuong M, Adams MJ, Kwong A, Haley CS, Amador C, McIntosh AM. Genome-by-trauma exposure interactions in adults with depression in the UK Biobank. JAMA Psychiatry. 2022;79:1110–7.
Hajat A, Nurius P, Song C. Differing trajectories of adversity over the life course: Implications for adult health and well-being. Child Abuse Negl. 2020;102:104392. https://doi.org/10.1016/j.chiabu.2020.104392
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779. https://doi.org/10.1371/journal.pmed.1001779
Mental health web-based questionnaire (Version 1.3). https://biobank.ctsu.ox.ac.uk/crystal/ukb/docs/mental_health_online.pdf. Accessed 15 July 2024.
Orellana SC, Bethlehem R, Simpson-Kent IL, van Harmelen AL, Vértes PE, Bullmore ET. Childhood maltreatment influences adult brain structure through its effects on immune, metabolic, and psychosocial factors. Proc Natl Acad Sci USA. 2024;121:e2304704121. https://doi.org/10.1073/pnas.2304704121
Bourassa KJ, Sbarra DA. Trauma, adversity, and biological aging: behavioral mechanisms relevant to treatment and theory. Transl Psychiatry. 2024;14:285. https://doi.org/10.1038/s41398-024-03004-9
Weller BE, Bowen NK, Faubert SJ. Latent class analysis: a guide to best practice. J Black Psychol. 2020;46:287–11.
Berlin KS, Williams NA, Parra GR. An introduction to latent variable mixture modeling (part 1): overview and cross-sectional latent class and latent profile analyses. J Pediatr Psychol. 2014;39:174–87.
Sinha P, Calfee CS, Delucchi KL. Practitioner’s guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. 2021;49:e63–e79.
Kongsted A, Nielsen AM. Latent class analysis in health research. J Physiother. 2017;63:55–58.
Grams ME, Rebholz CM, McMahon B, Whelton S, Ballew SH, Selvin E, et al. Identification of incident CKD stage 3 in research studies. Am J Kidney Dis. 2014;64:214–21.
Definitions of end stage renal disease (ESRD) for UK Biobank phase 1 outcomes adjudication. https://biobank.ndph.ox.ac.uk/showcase/refer.cgi?id=8319. Accessed 26 Nov 2023.
Razieh C, Zaccardi F, Miksza J, Davies MJ, Hansell AL, Khunti K, et al. Differences in the risk of cardiovascular disease across ethnic groups: UK Biobank observational study. Nutr Metab Cardiovasc Dis. 2022;32:2594–02.
Li R, Li R, Xie J, Chen J, Liu S, Pan A, et al. Associations of socioeconomic status and healthy lifestyle with incident early-onset and late-onset dementia: a prospective cohort study. Lancet Healthy Longev. 2023;4:e693–e702.
Yang G, Cao X, Li X, Zhang J, Ma C, Zhang N, et al. Association of unhealthy lifestyle and childhood adversity with acceleration of aging among UK Biobank participants. JAMA Netw Open. 2022;5:e2230690. https://doi.org/10.1001/jamanetworkopen.2022.30690
Cho S, Koyama S, Honigberg MC, Surakka I, Haidermota S, Ganesh S, et al. Genetic, sociodemographic, lifestyle, and clinical risk factors of recurrent coronary artery disease events: a population-based cohort study. Eur Heart J. 2023;44:3456–65.
Said MA, Verweij N, van der Harst P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank study. JAMA Cardiol. 2018;3:693–702.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Wuttke M, Li Y, Li M, Sieber KB, Feitosa MF, Gorski M, et al. A catalog of genetic loci associated with kidney function from analyses of a million individuals. Nat Genet. 2019;51:957–72.
Choi SW, Mak TS, O’Reilly PF. Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc. 2020;15:2759–72.
Li C, Chen Y, Chen Y, Ying Z, Hu Y, Kuang Y, et al. The causal association of irritable Bowel Syndrome with multiple disease outcomes: a phenome-wide mendelian randomization study. J Clin Med. 2023;12:1106. https://doi.org/10.3390/jcm12031106
Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, et al. Screening for lung cancer: US preventive services task force recommendation statement. JAMA. 2021;325:962–70.
Shi B, Choirat C, Coull BA, VanderWeele TJ, Valeri L. CMAverse: a suite of functions for reproducible causal mediation analyses. Epidemiology. 2021;32:e20–e22.
Kraft P, Yen YC, Stram DO, Morrison J, Gauderman WJ. Exploiting gene-environment interaction to detect genetic associations. Hum Hered. 2007;63:111–9.
Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. GigaScience. 2015;4:s13742-13015-0047–8. https://doi.org/10.1186/s13742-015-0047-8
Li C, Chen Y, Zhao W, Zhang C, Tang L, Ying Z, et al. Genetic impact on the association of sleep patterns and chronic kidney disease: a prospective cohort study of 157,175 UK Biobank participants. J Psychosom Res. 2023;169:111323. https://doi.org/10.1016/j.jpsychores.2023.111323
Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat Commun. 2017;8:1826. https://doi.org/10.1038/s41467-017-01261-5
Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet. 2000;25:25–9.
Liu H, Doke T, Guo D, Sheng X, Ma Z, Park J, et al. Epigenomic and transcriptomic analyses define core cell types, genes and targetable mechanisms for kidney disease. Nat Genet. 2022;54:950–62.
Sollis E, Mosaku A, Abid A, Buniello A, Cerezo M, Gil L, et al. The NHGRI-EBI GWAS Catalog: knowledgebase and deposition resource. Nucleic Acids Res. 2023;51:D977–85.
Surapaneni A, Schlosser P, Zhou L, Liu C, Chatterjee N, Arking DE, et al. Identification of 969 protein quantitative trait loci in an African American population with kidney disease attributed to hypertension. Kidney Int. 2022;102:1167–77.
Li J, Liu Z, Li M, Huang Y, Yin H, Xu G, et al. Associations of adverse childhood experiences with common psychiatric disorder in later life: results from the China mental health survey. BMC Geriatr. 2023;23:706. https://doi.org/10.1186/s12877-023-04421-z
Alcalá HE, Tomiyama AJ, von Ehrenstein OS. Gender differences in the association between adverse childhood experiences and cancer. Womens Health Iss. 2017;27:625–31.
Slopen N, Koenen KC, Kubzansky LD. Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: a systematic review. Brain Behav Immun. 2012;26:239–50.
Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21:642–9.
Thomas D. Gene-environment-wide association studies: emerging approaches. Nat Rev Genet. 2010;11:259–72.
Manning AK, Hivert MF, Scott RA, Grimsby JL, Bouatia-Naji N, Chen H, et al. A genome-wide approach accounting for body mass index identifies genetic variants influencing fasting glycemic traits and insulin resistance. Nat Genet. 2012;44:659–69.
Hancock DB, Soler Artigas M, Gharib SA, Henry A, Manichaikul A, Ramasamy A. et al. Genome-wide joint meta-analysis of SNP and SNP-by-smoking interaction identifies novel loci for pulmonary function. PLoS Genet. 2012;8:e1003098. https://doi.org/10.1371/journal.pgen.1003098.
Fan Q, Verhoeven VJ, Wojciechowski R, Barathi VA, Hysi PG, Guggenheim JA, et al. Meta-analysis of gene-environment-wide association scans accounting for education level identifies additional loci for refractive error. Nat Commun. 2016;7:11008. https://doi.org/10.1038/ncomms11008
Schunk SJ, Triem S, Schmit D, Zewinger S, Sarakpi T, Becker E, et al. Interleukin-1α Is a central regulator of leukocyte-endothelial adhesion in myocardial infarction and in chronic kidney disease. Circulation. 2021;144:893–908.
Frąk W, Kućmierz J, Szlagor M, Młynarska E, Rysz J, Franczyk B. New insights into molecular mechanisms of chronic kidney disease. Biomedicines. 2022;10:2846. https://doi.org/10.3390/biomedicines10112846
Yuan A, Lee Y, Choi U, Moeckel G, Karihaloo A. Chemokine receptor Cxcr4 contributes to kidney fibrosis via multiple effectors. Am J Physiol Renal Physiol. 2015;308:F459–72.
Tyra AT, Cook TE, Young DA, Hurley PE, Oosterhoff BJ, John-Henderson NA, et al. Adverse childhood experiences, sex, and cardiovascular habituation to repeated stress. Biol Psychol. 2021;165:108175. https://doi.org/10.1016/j.biopsycho.2021.108175
Bale TL, Epperson CN. Sex differences and stress across the lifespan. Nat Neurosci. 2015;18:1413–20.
Moody G, Cannings-John R, Hood K, Kemp A, Robling M. Establishing the international prevalence of self-reported child maltreatment: a systematic review by maltreatment type and gender. BMC Public Health. 2018;18:1164. https://doi.org/10.1186/s12889-018-6044-y
McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40:1647–58.
Tang L, Yang L, Chen W, Li C, Zeng Y, Yang H, et al. Sex-specific association between coffee consumption and incident chronic kidney disease: a population-based analysis of 359,906 participants from the UK Biobank. Chin Med J (Engl). 2022;135:1414–24.
Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. 2016;57:1103–12.
Patten SB, Wilkes TC, Williams JV, Lavorato DH, El-Guebaly N, Schopflocher D, et al. Retrospective and prospectively assessed childhood adversity in association with major depression, alcohol consumption and painful conditions. Epidemiol Psychiatr Sci. 2015;24:158–65.
Acknowledgements
This research has been conducted using the UK Biobank Resource under Application 54803. This work uses data provided by patients and collected by the NHS as part of their care and support. This research used data assets made available by National Safe Haven as part of the Data and Connectivity National Core Study, led by Health Data Research UK in partnership with the Office for National Statistics and funded by UK Research and Innovation (grant ref: MC_PC_20029 and MC_PC_20058). The research was funded by Key Research and Development Program of Chengdu (2021-YF08-00167-GX), the 1•3•5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18010), and Digital Economy Pilot Project for Application of Healthcare Big Data from National Development and Reform Commission of China (2018gfgw001).
Author information
Authors and Affiliations
Contributions
XZ, CL, JC, YC, HS conceived of and designed the study. CL, YC, and XZ performed data analyses. XZ, CL, CJ, and YC drafted the manuscript. CZ and HY contributed to the data cleansing and data management. XZ, SY, and PF provided important interpretation of the results from the clinical perspective. All authors contributed to the interpretation of the data, critically reviewed the manuscript, and approved the manuscript before submission for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The UK Biobank has obtained ethical approval from the NHS National Research Ethics Service (16/NW/0274). This study was approved by the Biomedical Research Ethics Committee of West China Hospital (2019-1171). All the UK Biobank participants gave written informed consent. The study was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, C., Chen, J., Chen, Y. et al. The association between patterns of exposure to adverse life events and the risk of chronic kidney disease: a prospective cohort study of 140,997 individuals. Transl Psychiatry 14, 424 (2024). https://doi.org/10.1038/s41398-024-03114-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-024-03114-4